There is no doubt that the 1918 Influenza Pandemic revolutionized public health and disease sciences for the better. And yet – despite the historical and scientific significance of this disastrous influenza, scientists struggled for decades to understand the true nature of the illness. Even today, while much has been discovered about the microorganism responsible for so much damage, much remains uncertain.
Defining: Virus
In 1918 and 1919, while Influenza ravaged global populations, scientists and public health officials struggled to comprehend the true mechanism behind the infections. Although basic principles of transmission were understood – well enough to encourage face coverings, personal hygiene, and quarantining – as science journalist Rose Rimler describes it, “they had the word, influenza, but they didn’t know exactly what a virus was – because they didn’t have microscopes that could see anything that small,” (Zuckerman 2020). The disease came and went before the pandemic virus could be understood, categorized, and preserved for future research. A decade after the end of the Influenza Pandemic, scientists discovered “an H1 subtype” of Haemophilus influenzae to be the “causative strain,” (Belser and Tumpey 2018, 255). While this discovery was certainly a landmark in understanding what truly happened in 1918, it left unanswered questions “regarding the extraordinary virulence and transmissibility” of the virus, (Belser and Tumpey 2018, 255). Furthermore, without any live viral particles preserved for research, such questions could not be answered until the virus could be reconstructed. And this was a hefty task given that by this point in scientific research, around the mid-1930s, all victims of the Influenza Pandemic had “either recovered, or they died,” (Zuckerman 2020).
Beyond the historical motivations for rebuilding the Influenza Pandemic of 1918, viral reconstruction was an imminent goal of public health officials. Rebuilding the virus would allow scientists to not only examine the properties of the illness in varying tissues but also to hopefully develop widespread influenza treatments that could save thousands of lives every flu season.
Recreating the Virus
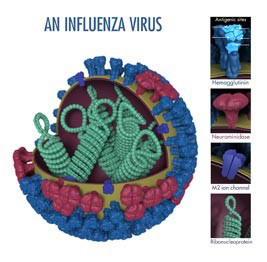
Image credits: The CDC
Thus began the journey to reconstruct the virus. In 1951, graduate student Johan Hultin traveled to Brevig Mission, Alaska, in hopes of discovering live viral particles in bodies buried in the Alaskan permafrost (Jordan 2019). Although Johan successfully uncovered influenza victims, still perfectly preserved in the permafrost, the lung tissue he carried back did not contain live viral particles (Zuckerman 2020). For decades, this seemed to be the last and only attempt to recover viral particles. However, upon the publication of Taunbenberger et al., 1997, which successfully sequenced 9 segments of RNA from the pandemic virus using victim lung tissue, the retired Hultin returned to Alaska to try to recover live samples again (Jordan 2019). This time, he managed to bring live viral particles in extracted lung tissue back to J.K. Tauberger and A.H. Reid. Within the next three years, researchers managed to fully sequence both the surface hemagglutinin (“HA”) gene and the neuraminidase (“NA”) gene. These discoveries would be critical to the ultimate recreation of the virus in the early 2000s.
In 2005, microbiologist Dr. Terrence Tumpey began his attempts to utilize this genome to construct a live replica of the influenza virus. The research itself was groundbreaking: using reverse genetics, Dr. Tumpey took the plasmids… for each of the 1918 viruses’ eight gene segments and inserted them into human kidney cells,” (Jordan 2019). These kidney cells would then integrate the gene segments into their nuclei and begin to synthesize the virus. Towards the end of July 2005, Dr. Tumpey managed to successfully rebuild the virus, and by August of that same year research was well underway. And, in the words of Dr. Tumpey and microbiologist Dr. Jessica A. Belser themselves, “Looking to the past, elucidating the role of specific molecular determinants that confer virulence and transmissibility of prior pandemic viruses is one approach. But we must also look to the future. Advances in next-generation sequencing are improving our understanding of virus diversity,” (Belser and Tumpey 2018, 255).
Uncertainty

Image credits: MSNBC
There is clearly much left to be determined about this devastating virus. For instance, there is still no conclusive evidence of the origins of the pandemic illness. Epidemiologists continue to publish differing theories of where the pandemic originated, with well-reasoned arguments supporting an origin in Haskell, Kansas as well as in rural South Asia. Scientists have also yet to uncover the biological basis for the different impacts of the various pandemic “waves.” As one study writes, “the exact origins of the fall virus, which was more lethal alone and more likely to be accompanied by bacterial pneumonia, are also unclear, but the most likely hypothesis is that a new strain arose in early August [1918] by genetic mutation or recombination in western France,” (Patterson and Pyle 1991, 8). Furthermore, “the extreme virulence of the fall wave has never been explained,” (Patterson and Pyle 1991, 4). The uncertainty shrouding the Influenza Pandemic, especially in light of the current public health catastrophe, serves “as a stark reminder of the continual threat influenza poses,” (Taubenberger and Morens 2019, 1). In fact, influenza attributed to the 1918 pandemic did not ever entirely disappear, but rather “went back to its usual pattern of regional epidemics of lesser virulence in the 1930s, 1040s, and early 1950s,” (Kilbourne 2006, 10). Genetic studies in the late 20th century confirmed this notion that the genes of the 1918 catastrophe remain present in daily life today; the “descendants of the 1918 virus remain today as annually circulating and evolving influenza viruses causing significant mortality each year,” (Taubenberger and Morens 2019, 1).
Thus, further pandemic preparedness remains a top priority for public health officials. The most obvious goal in pandemic preparedness is further understanding of the 1918 Influenza Pandemic. Answering questions of virulence, intensity, and origin could shed light on ways in which today’s society can adapt in anticipation of another influenza outbreak. With this understanding comes the potential for a “universal, broadly protective influenza vaccine for seasonal epidemics – a goal of intense research efforts,” (Belser and Tumpey 2018, 255). The development of more effective antiviral drugs would also greatly increase readiness in the event of another influenza pandemic.